The Subrogation Solution for Health Insurers and Health Plans
For nearly three decades, Intellivo has been setting the pace in health plan subrogation. It began with our founder helping lead the first arguments to the U.S. Supreme Court that laid the groundwork for subrogation law as we know it. Today, it continues with our technology-driven, client-first approach designed to capture maximum reimbursements while enhancing plan administration and protecting the experience of plan members.
Read on to see why the nation’s largest health plans and insurers rely on Intellivo.
-

Insurance Companies
Fully insured health plans face a patchwork of state-specific subrogation laws, each with its own protections, restrictions, and limitations. Intellivo technology and legal expertise ensure you don’t leave recoveries on the table or risk noncompliance…
-

Self-Funded Employers
Subrogation shouldn’t frustrate your employees. Intellivo replaces the outdated, intrusive questionnaire process with a seamless, technology-driven approach that eliminates confusion and reduces complaints…
-

Third-Party Administrators (TPAs)
Managing multiple health plans is complex. Subrogation doesn’t have to be. The right partner can lighten your team’s load and transform an operational task into a competitive differentiator…
-

Medicare Advantage Plans
Intellivo’s subrogation process is built for Medicare Advantage compliance. Our technology-driven approach identifies every potential recovery opportunity without burdening your members — ensuring you meet CMS expectations for coordination of benefits and avoid audit risk…
-

Medicaid Plans
Intellivo helps Medicaid Plans increase recoveries, ensure compliance and protect plan members. Traditional subrogation practices often come at the expense of member experience and compliance integrity. With Intellivo, Medicaid Plans can maintain both…
-

Taft-Hartley Plans
Union-affiliated health plans coast to coast trust Intellivo’s three decades of subrogation expertise. Protecting and supporting their plan members is the heart of their commitment, and ours…
-

Refer a case
Refer a new case or request a new case be opened…
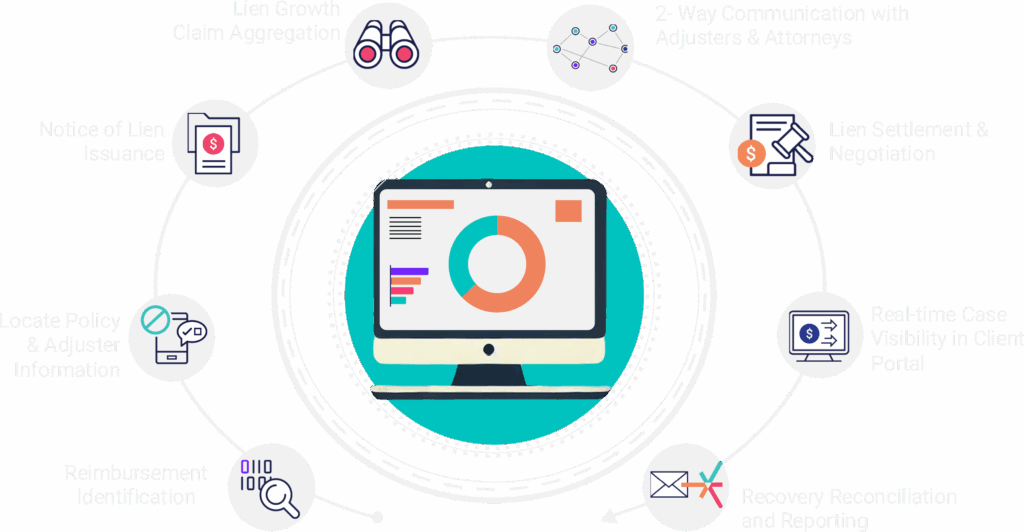
Intellivo’s Technology-Enabled Process
Recover More. Stress Less. Let’s Talk.
Subrogation doesn’t have to mean disruption. Intellivo delivers better results — for your plan, your team, and your members

